Function and diversity of HLA molecules
Human leukocyte antigen
Human leukocyte antigens (HLA) serve as recognition molecules, which allow our immune system to identify cells as part of the body. Our immune system is educated from childhood to tolerate cells as „self“ that present, like an identity card, the right HLA molecules on their surface. Cells that fail to present the right HLA molecules will be normally attacked by the immune system. HLA molecules structurally resemble small pockets, in which aberrant peptides are presented to highly educated immune cells, the so-called T lymphocytes or T cells. Whereas exogenous antigens are mostly presented by HLA class II molecules, expressed only on specialized, so-called antigen-presenting cells, the endogenous antigens, such as cancer antigens, are commonly presented by HLA class I molecules expressed on all nucleated cells.
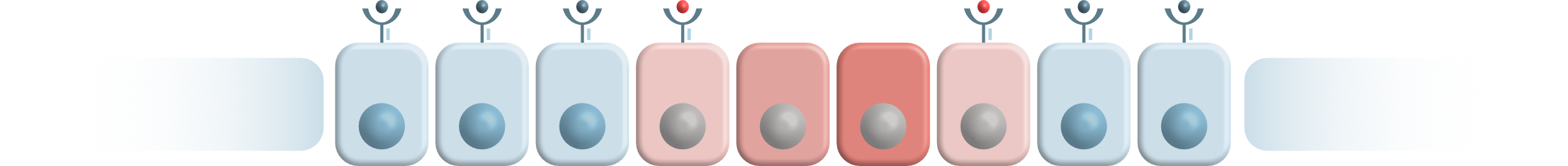
HLA molecules appear to be very diverse between different humans and different populations. In fact, there are over 20.000 distinct but related alleles. Every individual possesses a defined set of HLA molecules which implies only having a few different “pocket” shapes available. The diversity of HLA molecules has significant effects: Every HLA „pocket“ has a different shape and chemical property, allowing presentation only of certain structures. The immune system of an individual with a specific, fitting type of HLA molecule may effectively become alert against the presented antigen, whereas the immune system of an individual who has a non-fitting HLA molecule type, in contrast, may be „blind“ and unable to see antigen, as the pocket shape of the available HLA molecules may simply not fit. Thus, individuals with different HLA types might differently react to exactly the same virus, or have different courses of the same disease.
HLA molecules and Lynch syndrome
In contrast to most other cancers, tumors developing in Lynch syndrome carriers are full of structures that can potentially be recognized by the immune system. These so-called antigens or neoantigens result directly from mutations, which lead to tumor formation in Lynch syndrome. Although mutations are random and can occur everywhere in the genome during cell division, only certain mutations that enhance cells’ survival chance or fitness contribute to tumor development. The number of such survival-promoting mutations is low; therefore the pattern of mutations – and neoantigens – in Lynch syndrome tumors is shared among the tumors, and even among the patients.
Not all Lynch syndrome carriers develop tumors. In fact, only half of individuals who carry the genetic predisposition is affected by cancer associated with Lynch syndrome. Therefore, the question arises which is the factor determining that some patients develop cancer and some patients not.
It has been shown that immune cells already attack mutated cells in Lynch syndrome carriers before they develop manifest cancer. As the set of potential neoantigens in Lynch-Syndrome is very limited, it is possible that some HLA types are able to present a larger repertoire of abnormal peptides resulting in an increased immune response. This may lead to the situation that patient A, who has the same mutation profile as patient B, doesn’t develop cancer because all dangerous variants are already eliminated by the immune system, whereas patient B is affected by colorectal carcinoma. Referring to the three-phase-model of immune-editing, the patient’s HLA type could be the determining factor in Lynch syndrome, which can prevent the tumor cells from escaping the immune system.